AI Breaks In Healthcare.
Argo IQ Makes It Safe.
The control layer that verifies, monitors, and maintains the accuracy of AI-driven billing, eligibility, and intake workflows. Trusted by ops leaders where accuracy is revenue.



Healthcare is adopting AI faster than it can control it.
Automation is touching claims, eligibility, intake, documentation
— but none of it has a neutral QA layer.
Argo IQ is the independent verification layer healthcare has been missing.


We don’t automate healthcare workflows. We make sure your automations are right.
Observe Everything
Monitor every AI-driven workflow output
Verify & Fix
Detect errors, anomalies, missing fields
Human-in-loop
Verify with human-in-loop QA
Prove Accuracy
Maintain accuracy with continuous feedback

Argo IQ covers the top 80% of downstream denial risks — making sure they are correct.
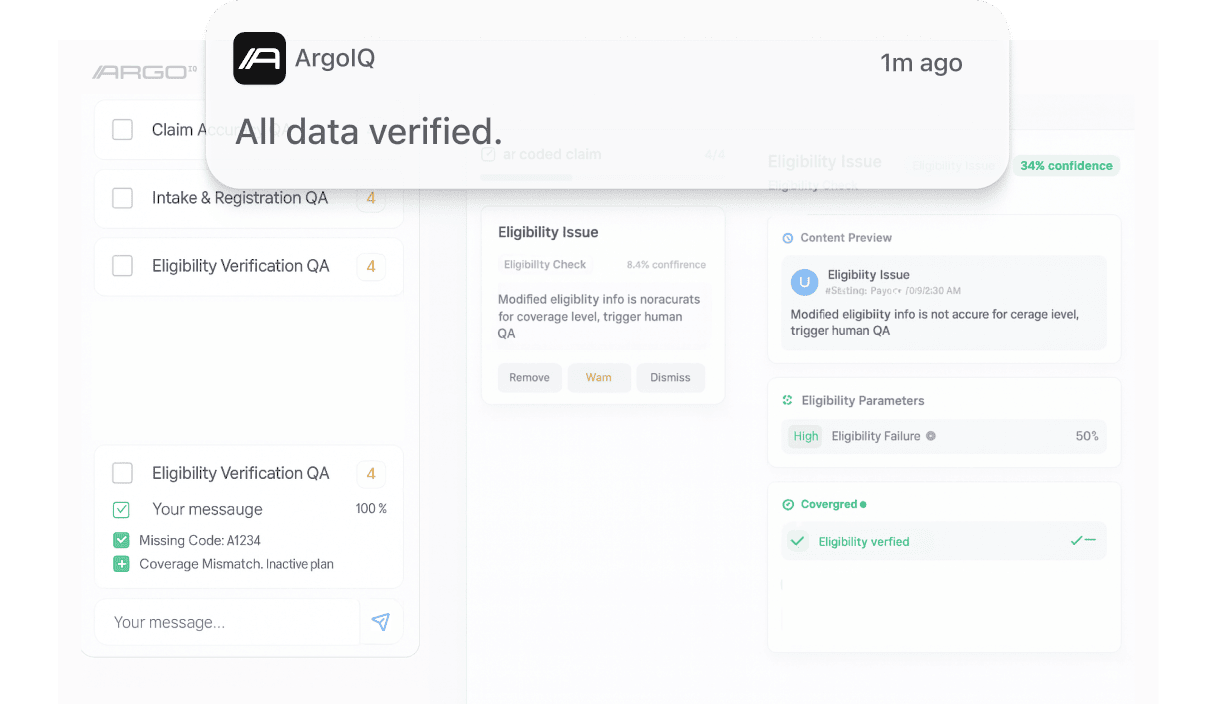
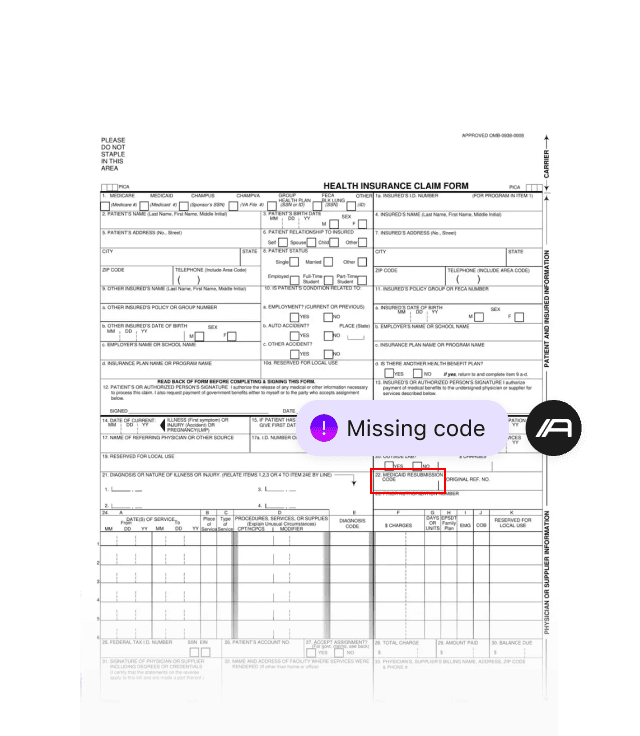
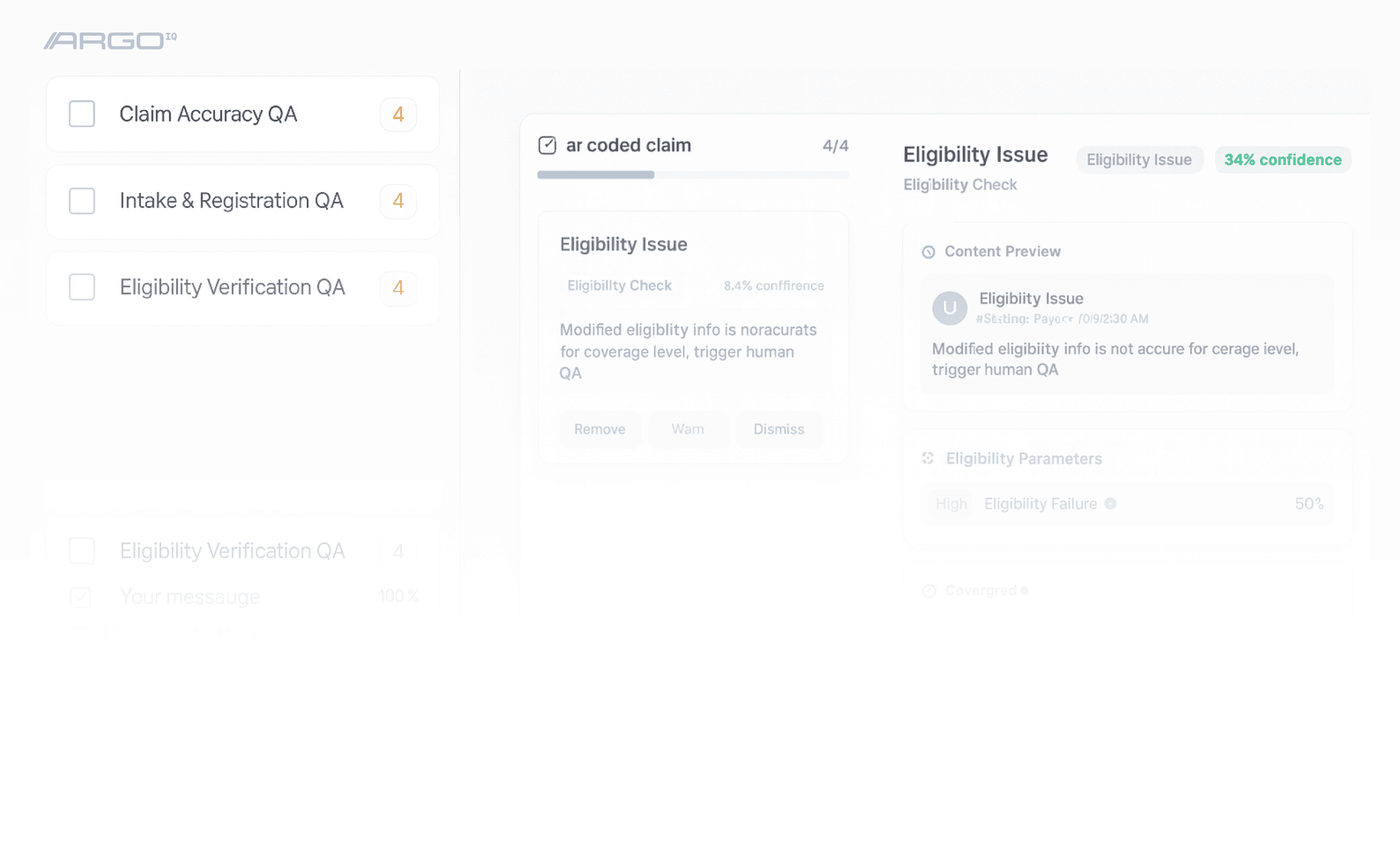
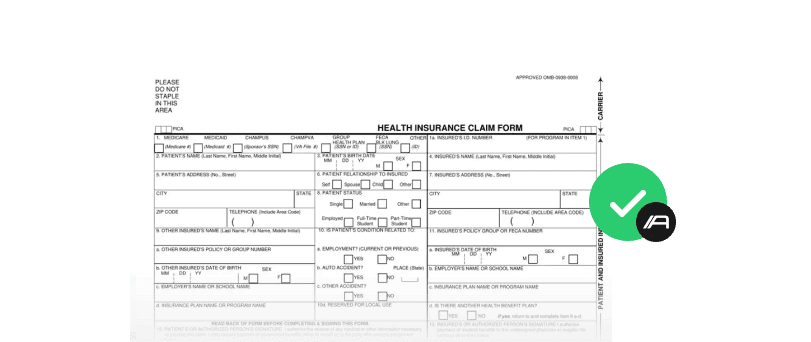
Claim Accuracy QA
Verify AI coded claims before submission. Catch missing codes, logic errors, and payer rules to cut denials and protect revenue.
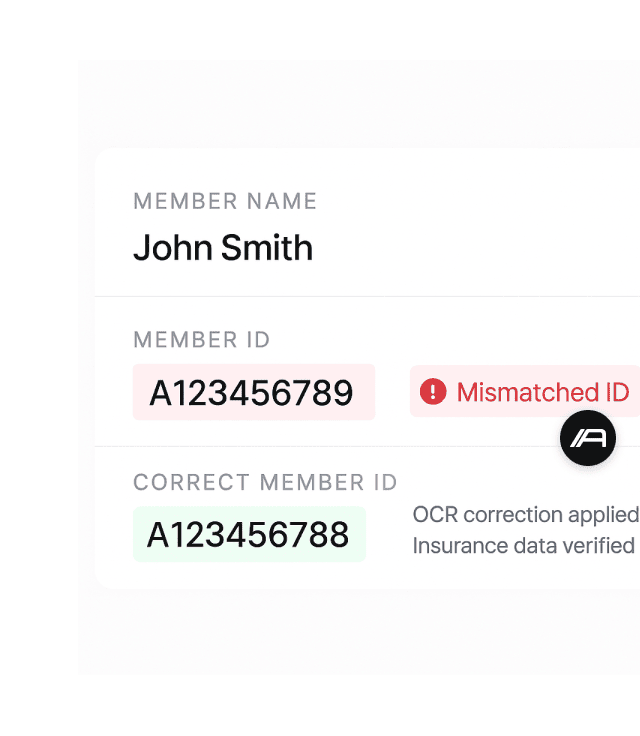
Eligibility Verification QA
Confirm eligibility data before it triggers denials. Validate payer responses, flag mismatches, and prevent cascading errors.
Argo IQ eliminates QA blind spots that automation creates.
hospital denials originate from eligibility & intake errors
Cost of rework caused by a single registration error.
Others run AI. Argo makes it correct.
AI builders automate. EHRs store data. RCM vendors process claims.
Argo verifies correctness.

Argo IQ monitors every run, flags anomalies, and routes to human QA for verifications.
You get verified outputs, clinical accuracy metrics, and audit trails that meet payer and compliance requirements.
Connect to your AI or RPA stack. Works with EHRs, clearinghouses, and eligibility systems.
Track every run and detect anomalies in real time for claims, eligibility checks, and intake data.
Route flagged items to Argo IQ’s QA team or your RCM analysts before claims move downstream.
See accuracy trends, denial risk, and operational savings in the dashboard.
Connect to your AI or RPA stack. Works with EHRs, clearinghouses, and eligibility systems.
Track every run and detect anomalies in real time for claims, eligibility checks, and intake data.
Route flagged items to Argo IQ’s QA team or your RCM analysts before claims move downstream.
See accuracy trends, denial risk, and operational savings in the dashboard.
Ingest AI output
Receive claim data, eligibility responses, or intake fields directly from your existing systems.
Detect anomalies / incorrect fields
Find missing codes, invalid insurance data, and payer rule mismatches before they trigger denials.
Route to Argo IQ QA reviewer
Trained analysts verify coding, confirm eligibility, and fix intake errors before claims move downstream.
Deliver corrected output
Clean, verified data flows back into your RCM, EHR, or billing system.
Continuous improvement
Low confidence? Edge case? Policy violation? Argo IQ routes the task to your team (or our vetted operator network) with full context. They complete it. Workflow continues.
Built for healthcare operators who need accuracy, not dashboards.
Revenue Cycle Management (RCM) Teams
Hospitals and RCM vendors dealing with denials, payer rules, and coding drift now have clean AI output, and verified claims.
Patient Access and Eligibility Teams
Hospitals, FQHCs, and ambulatory groups facing broken eligibility and wrong insurance data, now have accurate eligibility before billing.

Digital Health and Virtual Care Ops
Healthtech teams using AI for intake or documentation with inconsistent outputs can now work with verified, clinical quality data.
Where healthcare AI becomes accurate, auditable, and trusted.
Trusted by top operators building the future of AI and healthcare workflow accuracy.
Led by teams who scaled more than 2,000 human QA analysts across high stakes operations.
Full audit trails, verified outputs, and workflows built for claims, eligibility, and intake precision.
Healthcare ready verification for claims, intake data, and payer interactions where mistakes cost real money.

Your ROI is measured in fewer denials, cleaner data, and safer automation.